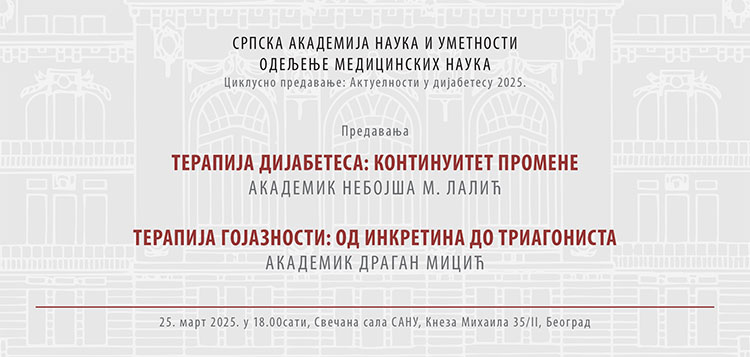
UPDATES IN DIABETES 2025 LECTURE SERIES OPENING
The lecture series titled ‘Updates in Diabetes 2025’ opens on Tuesday, 25 March, at 6 p.m. at the SASA Grand Hall. Academician Nebojša Lalić will deliver a lecture titled ‘Diabetes Treatments: The Continuity of Change’, whereas Academician Dragan D. Micić will give a lecture ‘Obesity Treatment: The Path from Incretins to Triagonists’.
Diabetes is one of the most prevalent non-infectious chronic diseases, which, according to the latest data, affects more than 530 million people (equivalent to one in ten individuals on the planet), while there is an estimation that the same number is at an increased risk of developing the disease. The situation is similar in Serbia, with an estimated 800.000 people (around 10% of the population) and the same number of people at risk. At the same time, and perhaps paradoxically, intensive research efforts utilizing sophisticated technology on large populations are being conducted to improve this growing health challenge. These research initiatives are highly complex and dynamic, bringing new and encouraging results practically every year that are integrated into diagnostics, treatment, and, to some extent, prevention.
Academician Nebojša M. Lalić, professor at the Faculty of Medicine, University of Belgrade, president of the Diabetes Association of Serbia, and president of the Executive Board of the International Diabetes Federation of Europe, will discuss the continuity of change in diabetes treatment.
As the lecture abstract states, in the last two decades, the results of intensive research in diabetes treatment have significantly expanded our understanding of new possibilities of optimal treatment leading to a rapid evolution in recommendations for contemporary therapy of type 2 diabetes (T2D). It has become evident that individual patient needs must be carefully considered when determining the optimal T2D therapy. This includes glycemic control, body weight management, and the presence or risk of complications such as cardiovascular diseases (CVDs) and diabetic kidney disease.
The latest recommendations for T2D treatment emphasize the importance of early intervention to prevent complications, bringing renewed focus to the choice of initial therapeutic agents, whether used alone or in combination.
As therapy further progresses, the new recommendations highlight the application of GLP-1 receptor agonists before insulin, although insulin therapy still remains the cornerstone of treatment, not only as a standalone option but also in combination with GLP-1 receptor agonists.
In type 1 diabetes (T1D), the past two decades have been characterized by not only a wide variety of new insulin formulations but also a significant advancement in insulin delivery technology and glycemia monitoring to enhance treatment outcomes.
One of the most notable breakthroughs is the confirmation of the benefits of continuous application of subcutaneous glucose sensors, which has contributed to the classification of insulin therapy success. The integration of insulin pumps with glucose sensors has paved the way for the routine use of hybrid artificial pancreas systems, offering promising new possibilities for improved disease management. There are also attempts at the application of glucose sensors—alone or in combination with insulin pumps—in type 2 diabetes (T2D) as well.
The second lecture titled ’Obesity Treatment: The Path from Incretins to Triagonists’ will be given by Academician Dragan D. Micić, secretary of the SASA Department of Medical Sciences in the third term, president of the Republic Expert Commission for Endocrinology and a member of the Council of the University of Belgrade.
As the lecture abstract outlines, the obesity epidemic, which started in the mid-1970s, has affected more than a billion people worldwide. The application of medicines modifying biological processes which influence appetite brings about weight loss and a considerable decrease in comorbidities associated with obesity.
Treatment of people with obesity problems includes pharmacological therapy combined with lifestyle changes (decreased intake of food and increase in physical activities). Obesity drugs can be categorized based on the mechanism of action into drugs that affect absorption in the gastrointestinal tract (Orlistat); centrally acting, appetite-modifying drugs (Phentermine-Topiramate and Naltrexone-Bupropionate), and drugs that mimic the action of enteropancreatic hormones that affect central appetite regulation and have multiple beneficial cardiometabolic benefits due to weight loss (Liraglutide, Semaglutide and Tirzepatide).
Incretins, gastrointestinal hormones that stimulate insulin secretion at physiological concentrations, have been a key focus in endocrinology for over a century. Research on incretins has led to the discovery of multiple gut hormones, some of which have agonists currently used in obesity therapy. New obesity drugs that are in various stages of preclinical and clinical trials include combinations of two or three agonists; combination of semaglutide 2.4 mg with cagrindide 2.4 mg (long-acting amylin analogue); survodutide (dual glucagon/GLP-1 receptor agonist); retatrudide (trireceptor agonist for GIP/GLP-1/glucagon.