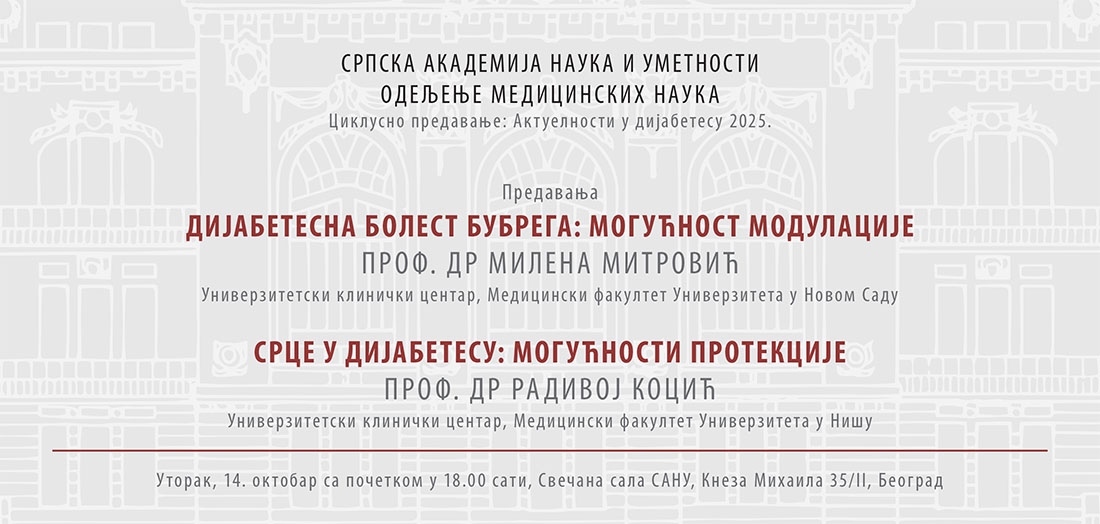
Updates in Diabetes 2025: Lectures by Professor Milena Mitrović, MD, and Professor Radivoj Kocić, MD
As part of the lecture series ’Updates in Diabetes 2025’, two lectures were delivered on Tuesday, 14 October, at the SASA Grand Hall. On this occasion, Professor Milena Mitrović, MD, gave a lecture titled ‘Diabetic Kidney Disease: Modulation Possibilities’, while Professor Radivoj Kocić, MD, discussed the topic ‘Heart in Diabetes: Prospects for Protection’.
According to Prof. Mitrović’s abstract, diabetic kidney disease represents one of the most common and most serious chronic complications of diabetes, occurring in approximately 20 to 40 per cent of patients, most frequently after fifteen to twenty years of disease duration. It is among the leading causes of end-stage renal failure, with nearly half of all patients starting hemodialysis having this condition as the underlying cause. In addition, diabetic kidney disease significantly increases the risk of cardiovascular morbidity and mortality, which is why a considerable number of patients pass away during the earlier stages of renal disease.
Diabetic kidney disease onset and its complications are influenced by multiple factors, with the most significant being hyperglycaemia, hypertension, disease duration, obesity, and genetic predisposition. In current diagnostic practice, two phenotypic forms are recognised: albuminuric and non-albuminuric, the latter of which is becoming increasingly prevalent among individuals with type 2 diabetes.
‘Contemporary guidelines underscore the importance of effective glycaemic control and optimal blood pressure management, alongside the use of contemporary renoprotective agents, which can slow disease progression and delay the need for dialysis,’ the lecture summary states.
Professor Radivoj Kocić, MD, delivered the second lecture titled ‘Heart in Diabetes: Prospects for Protection’.
Per Professor Kocić’s words, diabetes significantly accelerates the development of cardiovascular complications, often manifesting at earlier stages of life. Particularly concerning is that, over the past three decades, cardiovascular mortality among women with diabetes has risen by 23 per cent, whereas it has decreased by 27 per cent among women without diabetes.
Chronic heart failure (CHF) represents a common and serious complication of diabetes, marked by complex pathophysiological mechanisms involving dysfunction of the β₂-adrenergic and renin–angiotensin–aldosterone systems, as well as lipotoxicity, oxidative stress, chronic inflammation, and insulin resistance. Diabetic cardiomyopathy is seen as a special clinical entity, characterised by structural myocardial damage occurring independently of coronary artery disease.
Individuals with type 2 diabetes show a pronounced predisposition toward accelerated development of atherosclerosis and coronary ischemic disease, due to chronic hyperglycemia, dyslipidemia, insulin resistance, endothelial dysfunction, and inflammation. These factors jointly contribute to progressive vascular endothelial damage and the formation of atherosclerotic plaques. Silent myocardial ischemia in individuals with diabetes arises from a combination of autonomic neuropathy, microvascular dysfunction, and sympathetic nervous system hyperactivity, which leads to reduced pain perception and atypical clinical manifestations.
Professor Kocić will also talk about how artificial intelligence (AI) in contemporary clinical practice represents a key component of personalised medicine. Through sophisticated predictive analytics models, AI enables the early identification of cardiometabolic risk in individuals with type 2 diabetes. By integrating AI algorithms with data from continuous glucose monitoring (CGM) systems, wearable smart devices, and electronic health records, dynamic assessments of individual therapeutic responses, optimisation of antihyperglycemic therapy in real time, and adaptation of glycoregulatory strategies are achieved.
Not only does this technology enhance clinical screening and risk stratification, but it also supports proactive, data-driven decision-making, thereby significantly improving long-term outcomes in the prevention and treatment of diabetes-related cardiovascular complications.