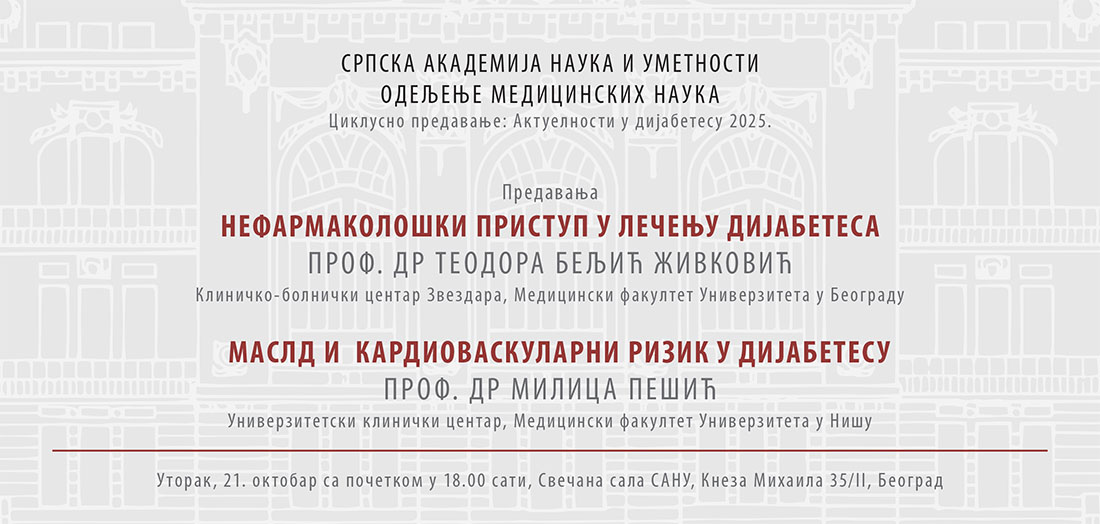
Updates in Diabetes 2025: Lectures by Professor Teodora Beljić Živković, MD, and Milica Pešić, MD
As part of the lecture series ’Updates in Diabetes 2025’, two lectures were delivered on Tuesday, 21 October, at the SASA Grand Hall. On this occasion, Professor Teodora Beljić Živković, MD, gave a lecture titled ‘Non-Pharmacological Method to Diabetes Treatment’, while Professor Milica Pešić, MD, discussed the topic ‘MASLD and Cardiovascular Risk in Diabetes’.
Professor Teodora Beljić Živković emphasised that individual medical nutritional therapy forms the foundation of diabetes treatment. It has been shown to improve glycemic control and insulin sensitivity, as well as to reduce diabetes-related complications, including obesity. In her lecture, she will discuss the types of diets recommended for individuals with diabetes and the importance of physical activity, which, together with medical nutritional therapy, is essential for both the prevention and treatment of diabetes.
People living with diabetes should have 150 minutes a week of moderate to strenuous aerobic activities, distributed in three non-consecutive days, along with two to three sessions of resistance exercises. Regular physical activity helps prevent the onset of diabetes and weight gain, and contributes to lowering blood pressure and blood lipid levels. Exercise recommendations should take into account physiological (reduced physical capacity, fatigue with minimal exertion), psychological (depression, diminished sense of self-worth), and therapeutic (adjustment of medication) barriers. Aerobic exercise improves capillary circulation and enhances glucose oxidation in muscles. It also enhances the activation of proteins participating in insulin signalisation, which in turn increases insulin sensitivity of the tissue, an effect that lasts up to 72 hours after exercising. Anaerobic exercises improve muscle strength due to an increase in GLUT-4 transporters, which enable a better glucose uptake in muscles. Exercising necessitates the integration of heart, muscles and blood vessels functions so that every improper activity can increase mortality risks. Therefore, a precise plan for physical activity must be prescribed, which depends on whether the goal is to improve body composition, reduce cardiovascular risks or recover from a cardiovascular event.’
The second lecture, titled ‘MASLD and Cardiovascular Risk in Diabetes’, was held by Professor Milica Pešić, MD.
’Metabolic dysfunction–associated steatotic liver disease (MASLD), previously known as non-alcoholic fatty liver disease (NAFLD), represents the most frequent chronic liver disease, particularly prevalent among individuals suffering from obesity and type 2 diabetes mellitus (T2DM). MASLD is not an isolated hepatic disease, but a systemic disorder which is closely linked to an increased risk of cardiovascular disease.. People suffering from MASLD and T2DM have a markedly higher probability of developing atherosclerotic disease, heart failure, atrial fibrillation, and overall cardiovascular mortality. The pathophysiological mechanisms connecting MASLD and cardiovascular disease include insulin resistance, systemic inflammation, dyslipidemia, oxidative stress, and endothelial dysfunction. Numerous pharmacological agents, including metformin, pioglitazone, GLP-1 receptor agonists, and SGLT2 inhibitors, target these shared pathophysiological mechanisms thereby not only do they improve the metabolic profile and liver condition, but also reduce cardiovascular risk. The bariatric surgery has also emerged as a highly effective approach in selected cases. The integration of MASLD into the assessment and management of cardiometabolic risk in people with T2DM becomes essential to the strategy of preventing complications and reducing mortality,’ explicates Professor Pešić in her abstract.